



Calluses

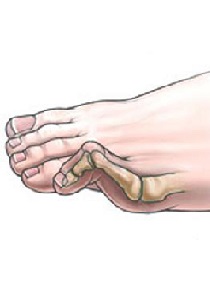
Bunion

Arthritis
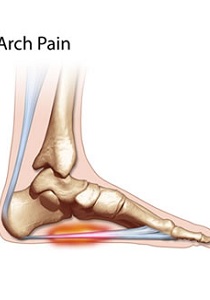
Arch Pain
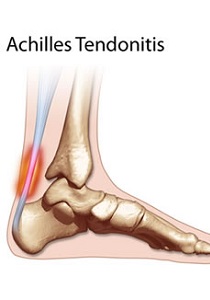
Achilles Tendonitis
Sesamoiditis

Shin Splints

Posterior Tibial Tendon Dysfunction

Plantar Fasciitis

Overlapping Toes

Over Pronation

Neuropathy

Mortons Toe

Mortons Neuroma
Mallet Toes
Metatarsalgia
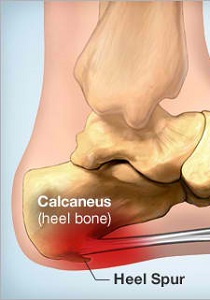
Heel Spur

Diabetic Foot

Corns
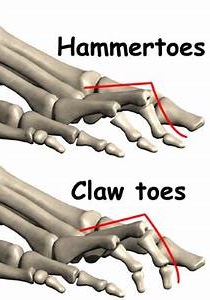
Claw/Hammer Toes

Charcot-Marie-Tooth

Calluses

Bunion

Arthritis
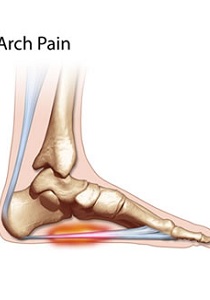
Arch Pain
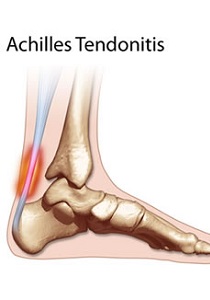
Achilles Tendonitis
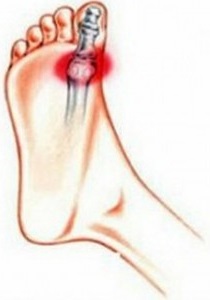
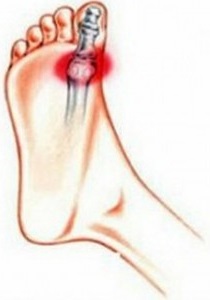
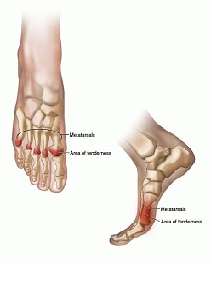
Sesamoiditis

Shin Splints

Posterior Tibial Tendon Dysfunction

Plantar Fasciitis

Overlapping Toes
Sesamoiditis is a common ailment that affects the forefoot, typically in young people who engage in physical activity like running or dancing. Its most common symptom is pain in the ball-of-the-foot, especially on the medial or inner side. The term is a general description for any irritation of the sesamoid bones, which are tiny bones within the tendons that run to the big toe. Like the kneecap, the sesamoids function as a pulley, increasing the leverage of the tendons controlling the toe. Every time you push off against the toe the sesamoids are involved, and eventually they can become irritated, even fractured. Because the bones are actually within the tendons, sesamoiditis is really a kind of tendinitis – the tendons around the bones become inflamed as well.
Sesamoiditis typically can be distinguished from other forefoot conditions by its gradual onset. The pain usually begins as a mild ache and increases gradually as the aggravating activity is continued. It may build to an intense throbbing. In most cases there is little or no bruising or redness. One of the major causes of sesamoiditis is increased activity. You’ve probably stepped up your activity level lately, which has forced you to put more pressure on the balls of your feet. Speedwork, hillwork, or even increased mileage can cause this. If you have a bony foot, you simply may not have enough fat on your foot to protect your tender sesamoids. Also, if you have a high arched foot, you will naturally run on the balls-of-your-feet, adding even more pressure.
Treatment for sesamoiditis is almost always noninvasive. Minor cases call for a strict period of rest, along with the use of a modified shoe or a shoe pad to reduce pressure on the affected area. This may be accomplished by placing a metatarsal pad away from the joint so that it redistributes the pressure of weight bearing to other parts of the forefoot. In addition, the big toe may be bound with tape or athletic strapping to immobilize the joint as much as possible and allow for healing to occur. It is recommended to decrease or stop activity for awhile. This will give your sesamoids time to heal. You should apply ice to the area for 10 to 15 minutes after exercise, or after any activity that aggravates the area. As with icing, anti-inflammatories will help the swelling go down so healing can begin. While the injury is healing, women should wear flat shoes on a daily basis.
Shin splints are a common lower extremity complaint, especially among runners and other athletes. They are characterized by pain in the front or inside aspect of the lower leg due to overexertion of the muscles. The pain usually develops gradually without a history of trauma, and might begin as a dull ache along the front or inside of the shin (Tibia) after running or even walking. Small bumps and tender areas may become evident adjacent to the shin bone. The pain can become more intense if not addressed, and shin splints should not be left untreated because of an increased risk of developing stress fractures. Shin splints usually involve small tears in the leg muscles where they are attached to the shin bone. The two types of shin splints are: anterior shin splints, in the front portion of the tibia; and posterior shin splints, occurring on the inside of the leg along the tibia.
Shin splints can be caused when the anterior leg muscles are stressed by running, especially on hard surfaces or extensively on the toes, or by sports that involve jumping. Wearing athletic shoes that are worn out or don’t have enough shock absorption can also cause this condition. Over-pronated (flat feet) are another factor that can lead to increased stress on the lower leg muscles during exercise. People with high arched feet can also experience shin splint discomfort because this foot type is a poor shock absorber.
The best way to prevent shin splints is to stretch and strengthen the leg muscles, wear footwear with good shock absorption, and avoid running on hard surfaces or excessive running or jumping on the ball-of-the-foot. Insoles or orthotics that offer arch support for over-pronation are also important. Treatment for shin splints should include taking a break from the exercise that is causing the problem until pain subsides. Icing the area immediately after running or other exercise can also be effective, along with gentle stretching before and after training. Another option is taking aspirin or ibuprofen to relieve pain and reduce inflammation. It is important not to try to train through the pain of shin splints. Runners should decrease mileage for about a week and avoid hills or hard surfaces. If a muscle imbalance, poor running form or flat feet are causing the problem, a long-term solution might involve a stretching and strengthening program and orthotics that support the foot and correct over-pronation. In more severe cases, ice, massage, electrostimuli, heat treatments and ultra-sound might be used.
Post-tib tendonitis is a strain placed on the posterior tibial tendon. The posterior tibial tendon runs along the inside of the ankle and the foot. When there is post-tibial tendon dysfunction, the tendon does not function to hold up the arch, resulting in flat feet. This can lead to heel pain, arch pain, plantar fasciitis and/or heel spurs. With post-tib tendonitis, pain will be more severe upon weight bearing, especially while walking or running.
Post-tib tendonitis occurs when the muscle is overused and the tendon (soft tissue) that connects the muscle to your bone is strained. Years of over-pronation (flat feet) can also lead to posterior tibial tendon dysfunction (PTTD). If you keep overusing the muscle, damage to the tendon builds up and tendonitis develops. At first the pain or swelling may come and go quickly, but eventually the problem may become more permanent.
To treat post-tib tendonitis, you can reduce your symptoms by limiting activity to control the pain and swelling. Stay off your feet a few days, then slowly increase your activity. Rest allows the tissues in your foot to heal. Conservative treatments (non-surgical treatments) include wearing a foot orthotic with rearfoot posting and longitudinal arch support to reduce strain on the post tibial tendon and prevent excessive stretching of the plantar fascia. The orthotic should also be designed with materials to comfort the foot and absorb shock. Listed below are tips to prevent post-tib tendonitis from recurring: Wear shoes that provide cushioning, support and shock absorption; Use orthotics with sufficient arch support that are constructed from shock absorbing, cushioning materials; Vary exercise routines, The variety will keep one set of muscles from being under continuous stress.
Plantar Fasciitis is an inflammation caused by excessive stretching of the plantar fascia. The plantar fascia is a broad band of fibrous tissue, which runs along the bottom surface of the foot, attaching at the bottom of the heel bone and extending to the forefoot. When the plantar fascia is excessively stretched, this can cause plantar fasciitis, which can also lead to heel pain, arch pain, and heel spurs.
Plantar Fasciitis often leads to heel pain, heel spurs, and/or arch pain. The excessive stretching of the plantar fascia that leads to the inflammation and discomfort can be caused by the following: Over-pronation (flat feet) which results in the arch collapsing upon weight bearing; A foot with an unusually high arch; A sudden increase in physical activity; Excessive weight on the foot, usually attributed to obesity or pregnancy; or Improperly fitting footwear. Over-pronation (flat feet) is the leading cause of plantar fasciitis. Over-pronation occurs in the walking process, when a person’s arch collapses upon weight bearing, causing the plantar fascia to be stretched away from the heel bone. With Plantar Fasciitis, the bottom of your foot usually hurts near the inside of the foot where the heel and arch meet. The pain is often acute either first thing in the morning or after a long rest, because while resting the plantar fascia contracts back to its original shape. As the day progresses and the plantar fascia continues to be stretched, the pain often subsides.
The key for the proper treatment of plantar fasciitis is determining what is causing the excessive stretching of the plantar fascia. When the cause is over-pronation (flat feet), an orthotic with rearfoot posting and longitudinal arch support is an effective device to reduce the over-pronation and allow the condition to heal. If you have unusually high arches, which can also lead to plantar fasciitis, cushion the heel, absorb shock and wear proper footwear that will accommodate and comfort the foot. Other common treatments include stretching exercises, plantar fasciitis night splints, wearing shoes that have a cushioned heel to absorb shock, and elevating the heel with the use of a heel cradle or heel cup. Heel cradles and heel cups provide extra comfort, cushion the heel, and reduce the amount of shock and shear forces placed during everyday activities. Every time your foot strikes the ground, the plantar fascia is stretched. You can reduce the strain and stress on the plantar fascia by following these simple instructions: Avoid running on hard or uneven ground, lose any excess weight and wear shoes and orthotics that support your arch to prevent over-stretching of the plantar fascia.
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. People of all ages can experience forefoot problems. Overlapping toes can occur in any of the toes and can cause extreme irritation if not corrected.
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. People of all ages can experience forefoot problems. Overlapping toes can occur in any of the toes and can cause extreme irritation if not corrected.
Any problems that cause pain or discomfort in the toes should be given prompt attention. Ignoring the symptoms can aggravate the condition, and lead to a breakdown of tissue or even infection. Conservative treatment (non-surgical treatment) of overlapping toes begins with accommodating the disorder. Shoes with a high, broad toe box (toe area) are recommended for people suffering from overlapping toes. Forefoot supports such as gel toe straighteners, gel toe caps and toe combs are often recommended to keep overlapping toes apart. These effective devices are designed to reduce friction to help relieve the discomfort.
Over-pronation, or flat feet, is a common biomechanical problem that occurs in the walking process when a person’s arch collapses upon weight bearing. This motion can cause extreme stress or inflammation on the plantar fascia, potentially causing severe discomfort and leading to other foot problems.
Over-pronation is very prominent in people who have flexible, flat feet. The framework of the foot begins to collapse, causing the foot to flatten and adding stress to other parts of the foot. As a result, over-pronation, often leads to Plantar Fasciitis, heel spurs, metatarsalgia, post-tib tendonitis and/or bunions. There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improperly fitting footwear can lead to additional foot problems.
Of the 16 million Americans with diabetes, 25% develop foot problems related to the disease. This is primarily due to a condition called neuropathy. Diabetic Neuropathy is a complication of diabetes that affects the nerves. The most common type of diabetic neuropathy is called peripheral neuropathy and affects the peripheral nerves. Peripheral nerves are the nerves that go out from the brain and spinal cord to the muscles, skin, internal organs, and glands. Peripheral neuropathy impairs proper functioning of these sensory and motor nerves. The most common symptoms of neuropathy include numbness and loss of feeling, usually in the feet and hands.
Diabetic Neuropathy can cause insensitivity or a loss of ability to feel pain, heat, and cold. Diabetics suffering from neuropathy can develop minor cuts, scrapes, blisters, or pressure sores that they may not be aware of due to the insensitivity. If these minor injuries are left untreated, complications may result and lead to ulceration, infection and possibly even amputation. Neuropathy can also cause deformities such as bunions, hammer toes, and Charcot feet. It is very important for diabetics to take the necessary precautions to prevent all foot-related injuries. Due to the consequences of neuropathy, daily observation of the feet is critical. When a diabetic patient takes the necessary preventative foot care measures, he or she reduces the risk of developing serious foot conditions.
The most successful way to prevent diabetic neuropathy from occurring is to control the diabetes. It is important to maintain blood sugars at normal levels and maintain normal blood pressure. In addition to this, it is important to:
Stop smoking
Limit the amount of alcohol you drink
Have regular physical exams
Have regular blood and urine tests
It is important for diabetics to treat their feet properly to avoid any future problems. Footwear and foot orthotics play an important role in diabetic foot care. Footwear that fits poorly can cause irritation and injury. Orthotics designed with Plastazote®, the #1 material for protecting the insensitive diabetic foot, are also frequently recommended. Plastazote is a material designed to accommodate pressure “hot spots” by conforming to heat and pressure. By customizing to the foot, Plastazote provides the comfort and protection needed in diabetic foot care. Footwear constructed with Plastazote is often recommended for the diabetic patient. Diabetic footwear should also provide the following benefits: High, wide toe box (high and wide space in the toe area); Removable insoles for fitting flexibility and the option to insert orthotics if necessary; Rocker soles, designed to reduce pressure in the areas of the foot most susceptible to pain, most notably the heel and the ball-of-the-foot; and Firm Heel Counters for extra and support and stability. It is important for diabetics with neuropathy to take the necessary precautions to prevent injury and keep their feet healthy.
Morton’s toe is a common forefoot disorder where the second toe is longer than the big toe (the Hallux).
Morton’s toe leads to excessive pressure on the second metatarsal head (behind the second toe at the ball-of-the-foot) resulting in pain similar to the discomfort associated with metatarsalgia. The constant pressure placed on the longer second toe while walking or standing can lead to callus formation under the second metatarsal head due to this excessive pressure.
Proper treatment of Morton’s toe starts with selecting proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating this condition. It may be necessary to buy footwear a half size to a size larger to accommodate the longer second toe. Orthotics that feature arch support to keep the foot aligned, and a metatarsal pad to reduce stress on the ball-of-the-foot are often recommended when treating this condition. Proper footwear combined with an effective orthotic will provide relief from pain associated with Morton’s toe.
Morton’s Neuroma is a common foot problem associated with pain, swelling and/or an inflammation of a nerve, usually at the ball-of-the-foot between the 3rd and 4th toes. Symptoms of this condition include sharp pain, burning, and even a lack of feeling in the affected area. Morton’s Neuroma may also cause numbness, tingling, or cramping in the forefoot.
Morton’s Neuroma is a foot condition caused from an abnormal function of the foot that leads to bones squeezing a nerve usually between the 3rd and 4th metatarsal heads. Symptoms of Morton’s Neuroma often occur during or after you have been placing significant pressure on the forefoot area, while walking, standing, jumping, or sprinting. This condition can also be caused by footwear selection. Footwear with pointed toes and/or high heels can often lead to a neuroma. Constricting shoes can pinch the nerve between the toes, causing discomfort and extreme pain.
The first step in treating Morton’s Neuroma is to select proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating and relieving the pain. The next step in treatment is to use an orthotic designed with a metatarsal pad. This pad is located behind the ball-of-the-foot to unload pressure, and relieve the pain caused by the neuroma.
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. A mallet toe occurs when the joint at the end of the toe cannot straighten. Excessive rubbing of the mallet toe against the top of the shoe can lead to pain and the development of a corn. The tip of the toe is often turned down against the shoe causing pressure and discomfort.
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. A mallet toe occurs when the joint at the end of the toe cannot straighten. Excessive rubbing of the mallet toe against the top of the shoe can lead to pain and the development of a corn. The tip of the toe is often turned down against the shoe causing pressure and discomfort. Arthritis can also lead to many forefoot deformities including mallet toes. Mallet toes can cause extreme discomfort, and can be aggravated if restrictive or improperly fitting footwear is worn for a prolonged period of time.
Any forefoot problems that cause pain or discomfort should be given prompt attention. Ignoring the symptoms can aggravate the condition and lead to a breakdown of tissue, or possibly even infection. Conservative treatment of mallet toes begins with accommodating the deformity. The goal is to relieve pressure, reduce friction, and transfer forces from the sensitive areas. Shoes with a high and broad toe box (toe area) are recommended for people suffering from forefoot deformities such as mallet toes. This prevents further irritation in the toe area from developing. Other conservative treatment includes forefoot supports such as gel toe caps, gel toe shields and toe crests. Gel forefoot supports provide immediate comfort and relief from common forefoot disorders without drying the skin.
Metatarsalgia is a general term used to denote a painful foot condition in the metatarsal region of the foot (the area just before the toes, more commonly referred to as the ball-of-the-foot). This is a common foot disorder that can affect the bones and joints at the ball-of-the-foot. Metatarsalgia (ball-of-foot-pain) is often located under the 2nd, 3rd, and 4th metatarsal heads, or more isolated at the first metatarsal head (near the big toe).
With this common foot condition, one or more of the metatarsal heads become painful and/or inflamed, usually due to excessive pressure over a long period of time. It is common to experience acute, recurrent, or chronic pain with metatarsalgia. Ball-of-foot pain is often caused from improper fitting footwear, most frequently by women’s dress shoes and other restrictive footwear. Footwear with a narrow toe box (toe area) forces the ball-of-foot area to be forced into a minimal amount of space. This can inhibit the walking process and lead to extreme discomfort in the forefoot. Other factors can cause excessive pressure in the ball-of-foot area that can result in metatarsalgia. These include shoes with heels that are too high or participating in high impact activities without proper footwear and/or orthotics. Also as we get older, the fat pad in our foot tends to thin out, making us much more susceptible to pain in the ball-of-the-foot.
The first step in treating metatarsalgia is to determine the cause of the pain. If improper fitting footwear is the cause of the pain, the footwear must be changed. Footwear designed with a high, wide toe box (toe area) and a rocker sole is ideal for treating metatarsalgia. The high, wide toe box allows the foot to spread out while the rocker sole reduces stress on the ball-of-the-foot. Unloading pressure to the ball-of-the-foot can be accomplished with a variety of foot care products. Orthotics designed to relieve ball-of-foot pain usually feature a metatarsal pad. The orthotic is constructed with the pad placed behind the ball-of-the-foot to relieve pressure and redistribute weight from the painful area to more tolerant areas. Other products often recommended include gel metatarsal cushions and metatarsal bandages. When these products are used with proper footwear, you should experience significant relief.
The heel bone is the largest bone in the foot and absorbs the most amount of shock and pressure. A heel spur develops as an abnormal growth of the heel bone. Calcium deposits form when the plantar fascia pulls away from the heel area, causing a bony protrusion, or heel spur to develop. The plantar fascia is a broad band of fibrous tissue located along the bottom surface of the foot that runs from the heel to the forefoot. Heel spurs can cause extreme pain in the rearfoot, especially while standing or walking.
Heel spurs develop as an abnormal growth in the heel bone due to calcium deposits that form when the plantar fascia pulls away from the heel. This stretching of the plantar fascia is usually the result of over-pronation (flat feet), but people with unusually high arches (pes cavus) can also develop heel spurs. Women have a significantly higher incidence of heel spurs due to the types of footwear often worn on a regular basis.
The key for the proper treatment of heel spurs is determining what is causing the excessive stretching of the plantar fascia. When the cause is over-pronation (flat feet), an orthotic with rearfoot posting and longitudinal arch support is an effective device to reduce the over-pronation, and allow the condition to heal. Other common treatments include stretching exercises, losing weight, wearing shoes that have a cushioned heel that absorbs shock, and elevating the heel with the use of a heel cradle, heel cup, or orthotic. Heel cradles and heel cups provide extra comfort and cushion to the heel, and reduce the amount of shock and shear forces experienced from everyday activities.
Diabetes is a serious disease that can develop from lack of insulin production in the body or due to the inability of the body’s insulin to perform its normal everyday functions. Insulin is a substance produced by the pancreas gland that helps process the food we eat and turn it into energy. Diabetes affects approximately 16 million Americans and is classified into 2 different types: Type 1 and Type 2. Type 1 is usually associated with juvenile diabetes and is often linked to heredity. Type 2, commonly referred to as adult onset diabetes, is characterized by elevated blood sugars, often in people who are overweight or have not attended to their diet properly. Many complications can be associated with diabetes. Diabetes disrupts the vascular system, affecting many areas of the body such as the eyes, kidneys, legs, and feet. People with diabetes should pay special attention to their feet.
Of the sixteen million Americans with diabetes, 25% will develop foot problems related to the disease. Diabetic foot conditions develop from a combination of causes including poor circulation and neuropathy. Diabetic Neuropathy can cause insensitivity or a loss of ability to feel pain, heat, and cold. Diabetics suffering from neuropathy can develop minor cuts, scrapes, blisters, or pressure sores that they may not be aware of due to the insensitivity. If these minor injuries are left untreated, complications may result and lead to ulceration and possibly even amputation. Neuropathy can also cause deformities such as bunions, hammer toes, and Charcot feet. It is very important for diabetics to take the necessary precautions to prevent all foot related injuries. Due to the consequences of neuropathy, daily observation of the feet is critical. When a diabetic patient takes the necessary preventative foot care measures, he or she reduces the risks of serious foot conditions.
Diabetes often leads to peripheral vascular disease that inhibits a person’s blood circulation. With this condition, there is a narrowing of the arteries that frequently leads to significantly decreased circulation in the lower part of the legs and the feet. Poor circulation contributes to diabetic foot problems by reducing the amount of oxygen and nutrition supplied to the skin and other tissue, causing injuries to heal poorly. Poor circulation can also lead to swelling and dryness of the foot. Preventing foot complications is more critical for the diabetic patient because poor circulation impairs the healing process and can lead to ulcers, infection, and other serious foot conditions.
Footwear and orthotics play an important role in diabetic foot care. Orthotics designed with Plastazote or P-Cell foam, the best materials for protecting the insensitive diabetic foot, are usually recommended. Plastazote is a material designed to accommodate pressure “hot spots” by conforming to heat and pressure. P-Cell functions the same but is designed for heavier patients. By customizing to the foot, Plastazote and P-Cell provide the comfort and protection needed in diabetic foot care. Footwear constructed with Plastazote is also recommended frequently for the diabetic patient. Diabetic footwear should also provide the following protective benefits:
High, wide toe box (high and wide space in the toe area)
Removable insoles for fitting flexibility and the option to insert orthotics if necessary.
Rocker Soles designed to reduce pressure in the areas of the foot most susceptible to pain, most notably the ball-of-the-foot.
Firm Heel Counters for support and stability.
If you are a diabetic, you should be particularly alert to any problems you may be having with your feet. It is very important for diabetics with neuropathy to take necessary precautions to prevent injury and keep their feet healthy. If you have diabetes and are experiencing a foot problem, immediately consult your foot doctor.
Proper foot care is especially critical for diabetics because they are prone to foot problems such as:
Loss of feeling in their feet
Changes in the shape of their feet
Foot ulcers or sores that do not heal
Simple daily foot care can prevent serious problems. According to the National Institute of Health, the following simple everyday steps will help prevent serious complications from diabetes:
Take Care of Your Diabetes Make healthy lifestyle choices to keep your blood sugar close to normal. Work with your health care team to create a diabetes plan that fits your lifestyle characteristics.
Check Your Feet Every Day You may have foot problems that you may not be aware of. Check your feet for cuts, sores, red spots, swelling, or infected toenails. Checking your feet should become part of your daily routine. If you have trouble bending over to see your feet, use a plastic mirror to help. You can also ask a family member to help you. Important Reminder: Be sure to call your doctor immediately if a cut, sore, blister, or bruise on your foot does not heal after one day.
Wash Your Feet Every Day Wash your feet in warm, NOT HOT, water. Do not soak your feet because your skin will get dry. Before bathing or showering, test the water to make sure it is not too hot. You should use a thermometer or your elbow. Dry your feet well. Be sure to dry between your toes. Use talcum powder to keep the skin dry between the toes.
Keep the Skin Soft and Smooth Rub a thin coat of skin lotion or cream on the tops and bottoms of the feet. Do not put lotion between your toes, because this might cause infection.
Wear Shoes and Socks At All Times Wear shoes and socks at all times. Do not walk barefoot, not even indoors. It is extremely easy to step on something and hurt your feet. Always wear seamless socks, stockings, and nylons with your shoes to help avoid the possibility of blisters and sores developing. Be sure to choose seamless socks that are made of materials that wick moisture away from your feet and absorb shock and shear. Socks made of these materials help keep your feet dry. Always check the insides of your shoes before putting them on. Make sure the lining is smooth and there are no foreign objects in the shoe, such as pebbles. Wear shoes that fit well and protect your feet.
Protect Your Feet From Hot and Cold Always wear shoes at the beach or on hot pavement. Put sunscreen on the tops of your feet for protection from the sun. Keep your feet away from radiators or open fires. DO NOT use hot water bottle or heating pads on your feet. If your feet are cold, wear seamless socks at night. Lined boots are good to keep your feet warm in the winter. Choose socks carefully. DO NOT wear socks with seams or bumpy areas. Choose padded socks to protect your feet and make walking more comfortable. In cold weather, check your feet often to keep your feet warm avoid frostbite.
Keep the Blood Flowing to Your Feet Put your feet up when you are sitting. Wiggle your toes for 5 minutes, 2 or 3 times a day. Move your ankles up and down and in and out to improve blood flow in your feet and legs.
DO NOT cross your legs for long periods of time.
DO NOT wear tight socks, elastic, or rubber bands, or garters around your legs.
DO NOT wear restrictive footwear or foot products. Diabetics should not wear foot products that can cut off circulation to the feet, such as products with elastic.
DO NOT smoke. Smoking reduces blood flow to your feet. If you have high blood pressure or high cholesterol, work with your health care team to lower it.
Be More Active Ask your doctor to plan an exercise program that is right for you. Walking, dancing, swimming, and bicycling are good forms of exercise that are easy on the feet. Avoid all activities that are hard on the feet, such as running and jumping. Always include a short warm-up or cool-down period. Wear protective walking or athletic shoes that fit well and offer good support.
Communicate With Your Doctor Ask your doctor to check the sense of feeling and pulses in your feet at least once a year. Ask your doctor to tell you immediately if you have serious foot problems. Ask your doctor for proper foot care tips and for the name of your local podiatrist.
Corns like calluses develop from an accumulation of dead skin cells on the foot, forming thick, hardened areas. They contain a cone-shaped core with a point that can press on a nerve below, causing pain. Corns are very common ailments that usually form on the tops, sides and tips of the toes. Corns can become inflamed due to constant friction and pressure from footwear. Corns that form between the toes are sometimes referred to as soft corns.
Some of the common causes of corn development are tight fitting footwear, high-heeled footwear, tight fitting stockings and socks, deformed toes, or the foot sliding forward in a shoe that fits too loosely. Soft corns result from bony prominences and are located between the toes. They become soft due to perspiration in the forefoot area. Complications that can arise from corns include bursitis and the development of an ulcer.
There are very simple ways to prevent and treat the corns. You should wear properly fitted footwear with extra room in the toe box (toe area). Avoid shoes that are too tight or too loose. Use an orthotic or shoe insert made with materials that will absorb shock and shear forces. Also avoid tight socks and stockings to provide a healthier environment for the foot. Try to steer away from corn removing solutions and medicated pads. These solutions can sometimes increase irritation and discomfort. Diabetics and all other individuals with poor circulation should never use any chemical agents to remove corns.
A claw toe is a toe that is contracted at the PIP and DIP joints (middle and end joints in the toe), and can lead to severe pressure and pain. Ligaments and tendons that have tightened cause the toe’s joints to curl downwards. Claw toes may occur in any toe, except the big toe. There is often discomfort at the top part of the toe that is rubbing against the shoe and at the end of the toe that is pressed against the bottom of the shoe. Claw toes are classified based on the mobility of the toe joints. There are two types – flexible and rigid. In a flexible claw toe, the joint has the ability to move. This type of claw toe can be straightened manually. A rigid claw toe does not have that same ability to move. Movement is very limited and can be extremely painful. This sometimes causes foot movement to become restricted leading to extra stress at the ball-of-the-foot, and possibly causing pain and the development of corns and calluses.
Claw toes result from a muscle imbalance, which causes the ligaments and tendons to become unnaturally tight. This results in the joints curling downwards. Arthritis can also lead to many different forefoot deformities, including claw toes.
Changing the type of footwear worn is a very important step in the treatment of claw toes. When choosing a shoe, make sure the toe box (toe area) is high and broad, and can accommodate the claw toes. A shoe with a high, broad toe box will provide enough room in the forefoot area so that there is less friction against the toes. Other conservative treatments include using forefoot products designed to relieve claw toes, such as toe crests and hammer toe splints. These devices will help hold down the claw toe and provide relief to the forefoot. Gel toe shields and gel toe caps are also recommended to eliminate friction between the shoe and the toe, while providing comfort and lubrication.
A hammer toe is a toe that is contracted at the PIP joint (middle joint in the toe), potentially leading to severe pressure and pain. Ligaments and tendons that have tightened cause the toe’s joints to curl downwards. Hammer toes may occur in any toe except the big toe. There is often discomfort at the top part of the toe due to rubbing against the shoe. Hammer toes are classified based on the mobility of the toe joints. There are two types – flexible and rigid. In a flexible hammer toe, the joint has the ability to move. This type of hammer toe can be straightened manually. A rigid hammer toe does not have that same ability to move. Movement is very limited and can be extremely painful. This sometimes causes foot movement to become restricted leading to extra stress at the ball-of-the-foot, and possibly causing pain and the development of corns and calluses.
Hammer toes result from a muscle imbalance, which causes the ligaments and tendons to become unnaturally tight. This results in the joint curling downward. Arthritis can also lead to many different forefoot deformities, including hammer toes.
Changing the type of footwear worn is a very important step in the treatment of hammer toes. When choosing a shoe, make sure the toe box (toe area) is high and broad, and can accommodate the hammer toes. A shoe with a high, broad toe box will provide enough room in the forefoot area so that there is less friction against the toes. Other conservative treatments include using forefoot products designed to relieve hammer toes, such as hammer toe crests and hammer toe splints. These devices will help hold down the hammer toe and provide relief to the forefoot. Gel toe shields and gel toe caps are also recommended to eliminate friction between the shoe and the toe, while providing comfort and lubrication.
Charcot-Marie-Tooth, or CMT, is inherited peripheral neuropathy and is found worldwide among all races and ethnic groups. Discovered in 1886 by three physicians, Jean-Martin Charcot, Pierre Marie, and Howard Henry Tooth, CMT affects an estimated 2.6 million people.
CMT usually isn’t life threatening and almost never affects brain function. It is not contagious, but it is hereditary and can be passed down from one generation to the next.
CMT patients slowly lose normal use of their extremities as nerves degenerate and muscles weaken because the affected nerves no longer stimulate the muscles. Many patients also have some loss of sensory nerve functions.
Although there are many different genetic causes of CMT, all types tend to have remarkably similar symptoms.
A high arched foot is generally one of the first signs of this disorder, although in some instances extremely flat feet are also typical of CMT.
As the disease progresses, structural foot deformities take place. The patient may develop a pes cavus (high-arched) foot and hammertoes.
The progressive muscle wasting of CMT also leads to problems with walking, running, and balance. Ankle weakness and sprains are common, and many patients develop foot drop.
Later in the course of the disease, hand function may become affected. Tasks requiring manual dexterity become difficult. The loss of nerve function is often accompanied by tingling and burning sensations in the hands and feet. This usually causes little more than mild discomfort, but some people experience severe neuropathic pain and require medication to control it.
Weakness of the respiratory muscles is rare in people with CMT, but when present, it can cause life-threatening problems. If shortness of breath is an issue, a patient should be checked by a respiratory specialist to see if the use of a ventilator is recommended.
It is important to note that the severity of symptoms can vary greatly from patient to patient, even within the same family. A child may or may not be more severely disabled than his/her parent. Some family members may experience significant impairment and require bracing while others have no noticeable symptoms but are found to have CMT upon examination by EMG or nerve conduction studies.
Although there is no cure for CMT at the present time, there are many therapies that can greatly improve life and function for CMT patients.
Physical therapy can maintain what movement, muscle strength and flexibility they have.
Many people benefit from occupational therapy which helps people accomplish the tasks of daily living with the use of assistive devices.
Bracing is another non-invasive form of correcting problems caused by CMT. Often gait abnormalities can be corrected by the use of either articulated (hinged) or unarticulated, molded braces called AFOs (ankle-foot orthoses). These braces help control foot drop and ankle instability and often provide a better sense of balance for patients.
Appropriate footwear is important for people with CMT, but they often have difficulty finding well-fitting shoes because of their high arched feet and hammered toes. Falls can generally be avoided by watching where one walks and by wearing appropriate footwear.
It is important for CMT patients to control their weight. Not only does extra weight make physical activity more difficult, but it also increases the stress on already compromised joints and muscles.
Patients should try to maintain as much strength and flexibility as possible. Generally, patients should consult a physical therapist or physician before beginning an exercise program, and avoid strenuous activity and overwork. Moderate activity and physical exercise can be beneficial, but patients must be conscious of their physical limitations.
Finally, stress management is important in maintaining a healthy body.
Any disabling condition can affect the way people think and feel about themselves, but having a chronic illness like CMT, which is often unseen, places stress on individuals and often causes depression. People with CMT can suffer from low self-esteem and relationships with others can be affected. Even when a person has learned to live with CMT, the progressive nature of the disorder may bring about more loss and the grieving process can begin again.
Some patients cope successfully on their own or with the support of family and friends; others find it therapeutic to talk to a professional counselor or to participate in a support group. To find additional information about CMT, please visit the CMTA’s website at cmtausa.org.
The formation of calluses is caused by an accumulation of dead skin cells that harden and thicken over an area of the foot. This callus formation is the body’s defense mechanism to protect the foot against excessive pressure and friction. Calluses are normally found on the ball-of-the-foot, the heel, and/or the inside of the big toe. Some calluses have a deep-seated core known as a nucleation. This particular type of callus can be especially painful to pressure. This condition is often referred to as Intractable Plantar Keratosis.
Calluses develop because of excessive pressure at a specific area of the foot. Some common causes of callus formation are high-heeled dress shoes, shoes that are too small, obesity, abnormalities in the gait cycle (walking motion), flat feet, high arched feet, bony prominences, and the loss of the fat pad on the bottom of the foot.
Many people try to alleviate the pain caused by calluses by cutting or trimming them with a razor blade or knife. This is not the way to properly treat calluses. This is very dangerous and can worsen the condition resulting in unnecessary injuries. Diabetics especially should never try this type of treatment. To relieve the excessive pressure that leads to callus formation, weight should be redistributed equally with the use of an orthotic. An effective orthotic transfers pressure away from the “hot spots” or high-pressured areas to allow the callus to heal. The orthotic should be made with materials that absorb shock and shear (friction) forces. Women should also steer away from wearing high-heeled shoes. As always, surgery should be the very last resort.
Bunions, referred to in the medical community as Hallux Valgus, are one of the most common forefoot problems. A bunion is a prominent bump on the inside of the foot around the big toe joint. This bump is actually a bone protruding towards the inside of the foot. With the continued movement of the big toe towards the smaller toes, it is common to find the big toe resting under or over the second toe. This causes a common forefoot condition called overlapping toes. Some of the symptoms of bunions include inflammation, swelling, and soreness on the side surface of the big toe. The discomfort commonly causes a patient to walk improperly.
Another type of bunion which some individuals experience is called a Tailor’s Bunion, also known as a Bunionette. This forms on the outside of the foot towards the joint at the little toe. It is a smaller bump that forms due to the little toe moving inwards, towards the big toe.
Bunions are a common problem experienced mostly by women. The deformity can develop from an abnormality in foot function, or arthritis, but is more commonly caused by wearing improper fitting footwear. Tight, narrow dress shoes with a constrictive toe box (toe area) can cause the foot to begin to take the shape of the shoe, leading to the formation of a bunion. Women who have bunions normally wear dress shoes that are too small for their feet. Their toes are squeezed together in their shoes causing the first metatarsal bone to protrude on the side of the foot.
It is important for men and women to realize that wearing dress shoes and boots, which are tapered in the toe area, can cause the bunion to worsen to the point where surgery is necessary.
In the early stages of the formation of a bunion, soaking feet in warm water can provide temporary relief. The best way to alleviate the pain associated with bunions is to wear properly fitting shoes. Shoes designed with a high, wide toe box (toe area) are recommended for people suffering from forefoot disorders, such as bunions. Shoes with rocker soles will unload pressure to the bunion area. Orthotics are also recommended for this condition to provide extra comfort, support, and protection.
Other conservative treatments include using forefoot products designed to accommodate and relieve bunions such as ((bunion shields, bunion night splints, and bunion bandages. These conservative treatments can limit the progression of the bunion formation, relieve pain and provide a healthy environment for the foot.
Arthritis is a disease characterized by the inflammation of the cartilage and lining of the body’s joints. Inflammation causes redness, warmth, pain and swelling. There are about 40 million Americans who suffer from arthritis. The National Institute of Arthritis and Musculoskeletal and Skin Diseases, estimates that by the year 2020, about 60 million Americans will have arthritis. The primary targets for arthritis are people over the age of 50. Arthritis is a major cause of foot pain because each foot has 33 joints that can become affected by the disease.
There are many different types of arthritis. The most common type is called osteoarthritis. Osteoarthritis causes excessive strain and the wearing away of cartilage in the joints of the foot. Movement becomes very difficult and painful. The pain and swelling worsens while standing or walking, and stiffness usually occurs after periods of rest.
Gout is another form of arthritis that also leads to foot complications. Excess uric acid crystals collect in and around the joints of the big toe. The big toe joint is commonly the focal point due to the stress and pressure it experiences during walking and other weight bearing activities. This often leads to severe pain in the big toe. Men are more likely to develop gouty arthritis than women.
Another type of arthritis is rheumatoid arthritis. It can develop at any age and there is no known cause for this condition. Rheumatoid arthritis is the most crippling form of the disease that can affect people of all ages. It can cause severe deformities of the joints with associated fatigue of the entire body. People who suffer from rheumatoid arthritis often develop severe forefoot problems such as bunions, hammer toes, claw toes, and others.
There are many causes of arthritis. Heredity plays a major role. However, arthritic symptoms can develop due to many other factors. Some of these include bacterial and viral infections, prescription and illegal drugs, traumatic injuries, and bowel disorders such as ileitis and colitis.
Forefoot problems such as hammer toes, claw toes, mallet toes, and bunions often develop as a result of arthritis, particularly Rheumatoid arthritis. Problems can also develop in the heel and ankle area due to the erosion of the involved joints.
Conservative treatment (non-surgical treatment) of the arthritic foot includes proper footwear, orthotics, and/or forefoot supports. Arthritic footwear should provide a high, wide toe box (high and wide space in the toe area). Removable insoles for fitting flexibility and the option to insert orthotics if necessary. Rocker Soles designed to facilitate ambulating (walking) and to reduce stress and pain at the ball-of-the-foot. Arthritic footwear should also accommodate swelling of the foot. Orthotics designed to provide comfort, support and extra cushioning are also recommended. Orthotics made with a material called Plastazote are often recommended because they mold to your feet to provide customized comfort. The proper footwear and orthotics will reduce pressure to provide a comfortable and healthy environment for the foot. Forefoot supports such as gel toe caps, gel toe shields, gel toe straighteners and others can often provide relief.
The term arch pain (often referred to as arch strain) refers to an inflammation and/or burning sensation at the arch of the foot.
There are many different factors that can cause arch pain. A structural imbalance or an injury to the foot can often be the direct cause. However, most frequently the cause is a common condition called plantar fasciitis. The plantar fascia is a broad band of fibrous tissue located along the bottom surface of the foot that runs from the heel to the forefoot. Excessive stretching of the plantar fascia, usually due to over-pronation (flat feet), causes plantar fasciitis. The inflammation caused by the plantar fascia being stretched away from the heel often leads to pain in the heel and arch areas. The pain is often extreme in the morning when an individual first gets out of bed or after a prolonged period of rest. If this condition is left untreated and strain on the longitudinal arch continues, a bony protrusion may develop, known as a heel spur. It is important to treat the condition promptly before it worsens.
This is a common foot condition that can be easily treated. If you suffer from arch pain avoid high-heeled shoes whenever possible. Try to choose footwear with a reasonable heel, soft leather uppers, shock absorbing soles and removable foot insoles. When the arch pain is pronation related (flat feet), an orthotic designed with a medial heel post and proper arch support is recommended for treating the pain. This type of orthotic will control over-pronation, support the arch and provide the necessary relief.
Achilles tendonitis causes inflammation and degeneration of the achilles tendon. The achilles tendon is the large tendon located in the back of the leg that inserts into the heel. The pain caused by achilles tendonitis can develop gradually without a history of trauma. The pain can be a shooting pain, burning pain or even an extremely piercing pain. Achilles tendonitis should not be left untreated due to the danger that the tendon can become weak and ruptured. Achilles tendonitis is aggravated by activities that repeatedly stress the tendon, causing inflammation. In some cases even prolonged periods of standing can cause symptoms. It is a common problem often experienced by athletes, particularly distance runners. Achilles tendonitis is a difficult injury to treat in athletes due to their high level of activity and reluctance to stop or slow down their training. Individuals who suffer from achilles tendonitis often complain that their first steps out of bed in the morning are extremely painful. Another common complaint is pain after steps are taken after long periods of sitting. This pain often lessens with activity.
There are several factors that can cause achilles tendonitis. The most common cause is over-pronation. Over-pronation occurs in the walking process, when the arch collapses upon weight bearing, adding stress on the achilles tendon. Other factors that lead to achilles tendonitis are improper shoe selection, inadequate stretching prior to engaging in athletics, a short achilles tendon, direct trauma (injury) to the tendon, and heel bone deformity.
Athletes, particularly runners, should incorporate a thorough stretching program to properly warm-up the muscles. They should decrease the distance of their walk or run, apply ice after the activity and avoid any uphill climbs. Athletes should use an orthotic device, heel cup, or heel cradle for extra support. A heel cup or heel cradle elevates the heel to reduce stress and pressure on the achilles tendon. The device should be made with light-weight, shock absorbing materials. An orthotic device can be used to control over-pronation, support the longitudinal arch, and reduce stress on the achilles tendon.
At Daily Living Medical Orthotics & Bracing, our focus is not only to provide our referral sources and patients with the care they deserve, but we also provide this service with unparalleled speed and accuracy while maintaining the most competitive prices. We only employ practitioners certified through the American Board for Certification in Orthotics and Prosthetics., and the Board of Certification/Accreditation (BOC).
Learn More
We’re happy to answer any questions you may have regarding our services or capabilities.
